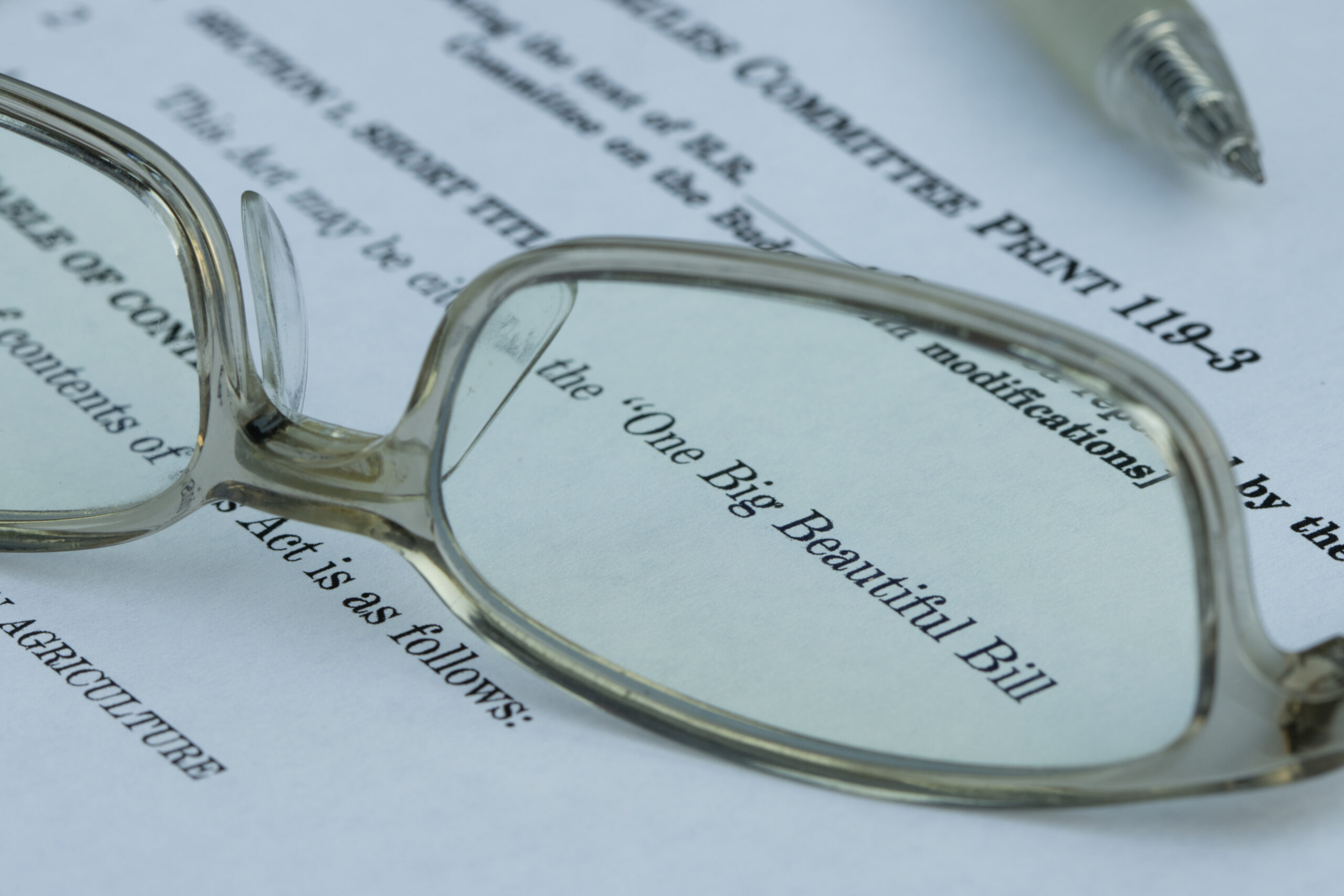
Understanding the New Medicare Advantage Reporting Requirement for Cost Reports
- Contributors
- Julia R. Jesuit
- W. Shane Hariel
Feb 16, 2026
Beginning with cost reporting periods ending on or after January 1, 2026, the Centers for Medicare & Medicaid Services (CMS) is introducing a new requirement for Medicare cost reports that will require significant preparation from hospitals and health systems. Under the recently finalized 2026 Outpatient Prospective Payment System (OPPS) rule, Medicare-certified acute care hospitals reimbursed under IPPS must begin reporting, on their annual cost reports, median negotiated payment rates from Medicare Advantage plans by Medicare Severity Diagnosis-Related Group (MS-DRG). This change reflects CMS’s evolving approach to rate setting and price transparency and carries both operational and strategic implications for providers.
What Changed and Why It Matters
Medicare cost reports have long been a key source of financial and utilization data that CMS uses for rate setting, research, and policy analysis. Traditionally, cost report data were based on standard fee-for-service rates and hospital cost distribution. With the updated reporting requirement, CMS is taking steps to incorporate information on negotiated rates actually paid by Medicare Advantage plans, which represent a growing share of inpatient payments. This data will support the development of MS-DRG relative weights beginning in fiscal year 2029, moving the rate-setting process closer to market-based payment dynamics. The use of the median payer-specific negotiated charges would replace the current use of gross charges that are reflected on a hospital’s chargemaster and cost information from Medicare cost reports for the development of the IPPS MS–DRG relative weights.
Because the Inpatient Prospective Payment System (IPPS) is budget-neutral, the new requirement will not directly increase overall Medicare spending. However, it may result in a redistribution of MS-DRG weights, potentially influencing relative payment rates across service groups and affecting hospital revenue and financial planning.
Who Must Comply
This reporting requirement applies to general acute care hospitals subject to IPPS in all 50 states, the District of Columbia, and Puerto Rico for cost reporting periods ending on or after January 1, 2026. Hospitals with fiscal year ends in early 2026 (for example, those with year-ends in January or February) will need to include this information on cost reports due in mid-2026.
Notably, the requirement does not apply to critical access hospitals, rural emergency hospitals or certain facilities that do not negotiate payment rates with Medicare Advantage plans (such as specific Indian Health Service hospitals or hospitals participating in Maryland’s Total Cost of Care Model during its performance period).
What Hospitals Must Report
CMS is introducing a new worksheet to capture this information – Worksheet S-12. Hospitals are required to report the median negotiated payment rate for each MS-DRG for which they have data in their most recent hospital price transparency machine-readable file (MRF). This includes:
- The median value of negotiated charges paid by Medicare Advantage plans for inpatient stays by MS-DRG; and
- Consistency of terminology and data sources across plans, discharges, and payment types.
If a hospital reports a specific dollar amount as a negotiated rate in its MRF, that amount should be used in the median calculation. If negotiated terms are reported as percentages or formula-based algorithms, hospitals must use the equivalent median allowed amount based on claim data. CMS also requires hospitals to exclude capitated payments and use established “crosswalk” processes to align non-standard payor discharges with MS-DRGs.
Since this reporting requirement entails a median, as opposed to average, rate, for each MS-DRG the provider will need to array all payment occurrences for the MS-DRG from lowest to highest to determine the median claim to determine the value to report.
CMS stated that further instructions for the reporting of the proposed market-based data collection requirement on the Medicare cost report would be discussed in a forthcoming new Information Collection Request.
Operational and Compliance Considerations
This new reporting requirement introduces both compliance risk and operational complexity. The calculation of a weighted median negotiated rate requires hospitals to coordinate data from multiple sources, including:
- The price transparency MRF, which lists Medicare Advantage payor-specific negotiated payment data,
- Internal discharge and claims records,
- Electronic remittance data (such as EDI 835 electronic remittance advice),
- Tools and processes to accurately assign discharges to the appropriate MS-DRGs.
Hospitals will need to assemble cross-functional teams — including revenue cycle, managed care contracting, finance, and compliance — to gather, validate, and reconcile these data elements. The time and labor needed to meet reporting expectations may exceed CMS’s initial estimates, so thoughtful planning and resource allocation are critical.
Strategic Implications
Though the requirement adds reporting obligations, it also offers insights that hospitals can use strategically. Once incorporated into the Healthcare Provider Cost Reporting Information System (HCRIS), these median negotiated rate data will allow hospitals to benchmark their performance against peer organizations. Early analysis may reveal whether an organization’s contractual terms with Medicare Advantage plans are favorable relative to market norms or warrant adjustments in future negotiations.
Because many Medicare Advantage negotiated rates today align closely with traditional fee-for-service rates — but may be tempered by denials, edits, or coding practices — the resulting median values may provide important visibility into actual reimbursement trends and opportunities for optimization.
Preparing for Implementation
To prepare effectively, hospitals should:
- Develop a comprehensive understanding of the final OPPS rule and the associated cost report worksheet structure,
- Allocate sufficient time and staff to capture, calculate, and reconcile negotiated rate data, and
- Engage revenue cycle, managed care, and finance teams early in the process to align internal systems and reporting practices.
Partnering with external advisors or consultants can also help ensure that assumptions, source data, and calculations are defensible and consistent with CMS expectations.
Next Steps for Hospitals and Health Systems
The addition of Medicare Advantage negotiated rate reporting represents an important shift in Medicare cost reporting and reflects CMS’s broader focus on market-driven payment data. Hospitals that proactively prepare and coordinate across departments will be better positioned to comply with the new requirement and leverage the resulting data for strategic insights into reimbursement trends.
If you have questions about this new Medicare Advantage negotiated rate reporting requirement or want help assessing its impact on your cost reporting processes and financial planning, contact your CRI advisor. Proactive engagement now can help ensure compliance and position your organization for long-term operational success.